Cholerhiasis might sound like a fancy dish you’d find in a five-star restaurant, but it’s actually a serious condition that can leave anyone feeling less than fabulous. Imagine your gallbladder throwing a tantrum because it can’t handle the cholesterol overload. That’s cholerhiasis for you—gallstones galore!
With the potential to turn a simple meal into a painful episode, understanding this condition is crucial. It’s not just about avoiding that extra slice of pizza; it’s about keeping your digestive system happy and functioning smoothly. So, buckle up as we dive into the world of cholerhiasis, where knowledge can help prevent those pesky gallstones from crashing the party.
Table of Contents
ToggleOverview of Cholerhiasis
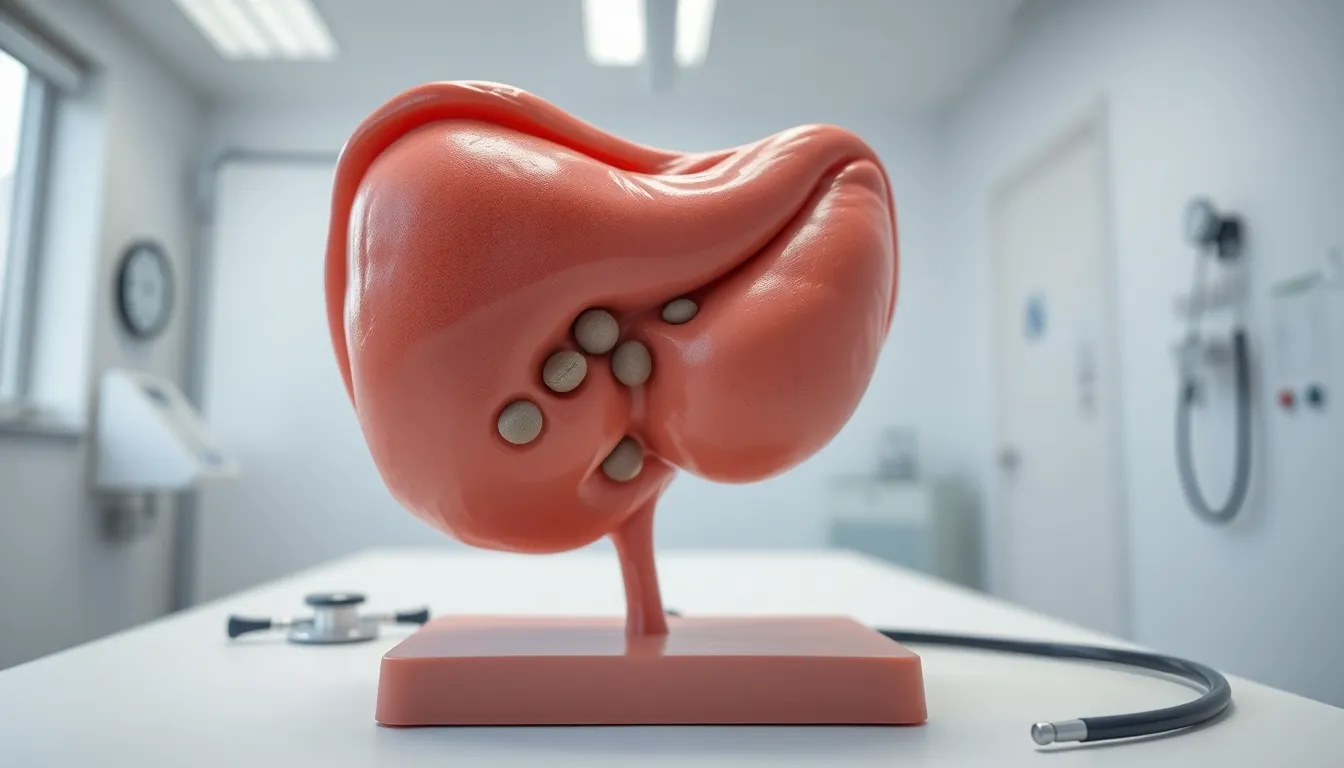
Cholerhiasis signifies the presence of gallstones primarily composed of cholesterol. This condition arises when excess cholesterol accumulates in the gallbladder, leading to painful complications during digestion.
Definition of Cholerhiasis
Cholerhiasis refers to the formation of cholesterol gallstones in the gallbladder. These stones develop when there’s an imbalance in the substances that make up bile, particularly when cholesterol exceeds the bile’s ability to dissolve it. Gallstones can vary in size, and their presence often leads to blockages, causing acute discomfort.
Causes and Risk Factors
Multiple factors contribute to the development of cholerhiasis. Obesity ranks as a significant risk factor, as excess weight elevates cholesterol levels. Additionally, age plays a role; individuals over 40 exhibit higher prevalence rates. Family history also influences risk, with genetic predispositions making some individuals more susceptible. Diets high in fat and low in fiber further increase chances. Lack of physical activity compounds these risks, leading to a greater likelihood of gallstone formation.
Symptoms of Cholerhiasis

Recognizing the symptoms of cholerhiasis is crucial for timely intervention. Symptoms can range from mild to severe, impacting daily life.
Common Symptoms
Individuals often report intermittent pain in the upper right abdomen. Bloating frequently accompanies this discomfort after meals. Nausea may also occur, particularly following fatty foods. An individual might experience vomiting, which can exacerbate feelings of queasiness. Many patients describe changes in digestive habits, such as increased gas or indigestion. Some may notice weight fluctuations due to dietary restrictions or discomfort.
Severe Symptoms
Intense abdominal pain can signify a blockage caused by gallstones. This pain often radiates to the back or right shoulder. Fever and chills may develop, indicating a potential infection or inflammation. Significant jaundice, or yellowing of the skin, can occur when bile ducts are obstructed. Changes in urine color or stool can signal serious complications, alerting individuals to seek immediate medical attention. Sudden onset of severe symptoms requires immediate evaluation by healthcare professionals.
Diagnosis of Cholerhiasis
Diagnosing cholerhiasis involves a combination of medical history assessment and physical examination, alongside advanced diagnostic tests to confirm gallstone formation.
Medical History and Physical Examination
A healthcare provider starts with a thorough medical history, focusing on symptoms, risk factors, and dietary habits. Specific attention is paid to the patient’s age, weight, and any family history of gallstones. They inquire about the frequency, duration, and intensity of abdominal pain experienced. A physical exam may reveal tenderness in the upper right abdomen, often indicating inflamed gallbladder or surrounding tissues. This initial evaluation helps identify potential complications caused by gallstones.
Diagnostic Tests
To confirm a diagnosis, several diagnostic tests are utilized. Abdominal ultrasound remains the primary method due to its accuracy in detecting gallstones. Moreover, a computed tomography (CT) scan can provide detailed images, identifying complications such as inflammation. Magnetic resonance cholangiopancreatography (MRCP) is another non-invasive imaging technique that visualizes the bile ducts. Blood tests may assess liver function and any signs of infection. Collectively, these tests guide healthcare providers in developing an effective treatment plan.
Treatment Options for Cholerhiasis
Various treatment options exist for cholerhiasis, addressing both symptoms and the underlying condition. These treatments vary based on severity and individual patient needs.
Non-Surgical Treatments
Lifestyle modifications play a crucial role in managing cholerhiasis. A diet low in saturated fats and high in fiber helps reduce cholesterol levels. Medications such as ursodeoxycholic acid facilitate the dissolution of gallstones in select patients. These treatments target gallstones and prevent further formation. Regular physical activity, such as walking or swimming, enhances gallbladder function and decreases the risk of gallstone complications. Avoiding rapid weight loss also contributes significantly, as it can lead to increased cholesterol synthesis.
Surgical Treatments
When non-surgical interventions fail to alleviate symptoms, surgical options become necessary. Cholecystectomy, the removal of the gallbladder, remains the most common surgical procedure for cholerhiasis. Surgeons often perform this operation laparoscopically, minimizing recovery time. In some cases, endoscopic retrograde cholangiopancreatography (ERCP) assists in removing stones obstructing the bile duct. Surgical choices depend on the patient’s overall health, gallstone size, and potential complications. Regular follow-up consultations ensure a comprehensive approach to managing cholerhiasis and preventing recurrence.
Prevention of Cholerhiasis
Maintaining a healthy lifestyle significantly reduces the risk of cholerhiasis. Consuming a diet rich in fruits, vegetables, and whole grains supports digestive health and helps regulate cholesterol levels. Foods high in fiber, such as oats, beans, and nuts, are essential in minimizing cholesterol absorption in the body.
Regular physical activity plays a key role in preventing gallstone formation. Engaging in moderate exercise, like walking, swimming, or cycling for at least 150 minutes weekly, aids weight management and boosts overall health. Sedentary lifestyles contribute to obesity, which increases the likelihood of gallstone development.
Hydration remains crucial in maintaining proper bile function. Drinking sufficient water throughout the day ensures that bile remains fluid, helping to dissolve cholesterol and prevent stone formation. Recommended intake usually ranges between 8 to 10 cups of water daily.
Controlling body weight helps minimize gallstone risks. A gradual weight loss approach is preferable, aiming for 1 to 2 pounds per week, to avoid the rapid loss that may increase cholesterol saturation in bile. Sustainable dietary choices rather than extreme diets contribute to effective weight management.
Limiting saturated fats and avoiding refined carbohydrates are essential dietary strategies. High-fat foods, like fried items and processed snacks, should be consumed in moderation. Prioritizing healthy fats, such as those found in fish, avocados, and olive oil, can support bile health.
Periodic medical check-ups assist in identifying risk factors early. Health professionals can evaluate lipid levels, provide dietary guidance, and offer individualized recommendations. Taking preventative measures significantly aids in reducing the likelihood of developing cholerhiasis.
Cholerhiasis poses significant challenges for those affected by it. Understanding the condition and its symptoms is essential for early diagnosis and effective management. By adopting a healthy lifestyle that includes a balanced diet and regular exercise individuals can significantly reduce their risk of developing gallstones.
Timely medical intervention can alleviate severe symptoms and prevent complications. With the right strategies in place individuals can maintain their digestive health and minimize the impact of cholerhiasis on their daily lives. Regular follow-ups with healthcare providers ensure ongoing support and tailored advice for managing this condition effectively.